Bsc Classification
Balanced Scorecard Templates Classification Using a template is an excellent way to get started easily. In the case of the Balanced Scorecard the topic of the template might be something complicated because the key idea about this concept is not in rectangle diagram, or simply grouping metrics into four perspectives.
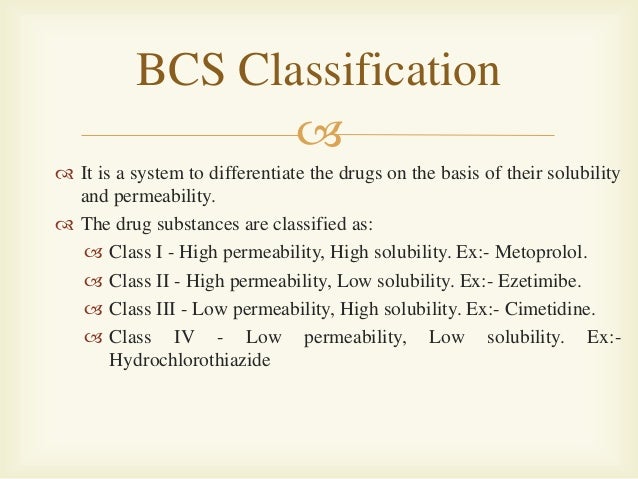
The Biopharmaceutics Classification System is a system to differentiate the drugs on the basis of their solubility and permeability.[1]

This system restricts the prediction using the parameters solubility and intestinal permeability. The solubility classification is based on a United States Pharmacopoeia (USP) aperture. The intestinal permeability classification is based on a comparison to the intravenous injection. All those factors are highly important because 85% of the most sold drugs in the United States and Europe are orally administered[citation needed].
BCS classes[edit]
According to the Biopharmaceutical Classification System (BCS) drug substances are classified to four classes upon their solubility and permeability:[1]
- Class I - high permeability, high solubility
- Example: metoprolol, paracetamol[2]
- Those compounds are well absorbed and their absorption rate is usually higher than excretion.
- Class II - high permeability, low solubility
- Example: glibenclamide, bicalutamide, ezetimibe, aceclofenac
- The bioavailability of those products is limited by their solvation rate. A correlation between the in vivo bioavailability and the in vitro solvation can be found.
- Class III - low permeability, high solubility
- Example: cimetidine
- The absorption is limited by the permeation rate but the drug is solvated very fast. If the formulation does not change the permeability or gastro-intestinal duration time, then class I criteria can be applied.
- Class IV - low permeability, low solubility
- Example: Bifonazole
- Those compounds have a poor bioavailability. Usually they are not well absorbed over the intestinal mucosa and a high variability is expected.
Definitions[edit]
The drugs are classified in BCS on the basis of solubility, permeability, and dissolution.
Solubility class boundaries are based on the highest dose strength of an immediate release product. A drug is considered highly soluble when the highest dose strength is soluble in 250 ml or less of aqueous media over the pH range of 1 to 7.5. The volume estimate of 250 ml is derived from typical bioequivalence study protocols that prescribe administration of a drug product to fasting human volunteers with a glass of water.
Permeability class boundaries are based indirectly on the extent of absorption of a drug substance in humans and directly on the measurement of rates of mass transfer across human intestinal membrane. Alternatively non-human systems capable of predicting drug absorption in humans can be used (such as in-vitro culture methods). A drug substance is considered highly permeable when the extent of absorption in humans is determined to be 90% or more of the administered dose based on a mass-balance determination or in comparison to an intravenous dose.
For dissolution class boundaries, an immediate release product is considered rapidly dissolving when no less than 85% of the labeled amount of the drug substance dissolves within 15 minutes using USP Dissolution Apparatus 1 at 100 RPM or Apparatus 2 at 50 RPM in a volume of 900 ml or less in the following media: 0.1 N HCl or simulated gastric fluid or pH 4.5 buffer and pH 6.8 buffer or simulated intestinal fluid.
See also[edit]
- ADME
References[edit]
- ^ abMehta M (2016). Biopharmaceutics Classification System (BCS): Development, Implementation, and Growth. Wiley. ISBN978-1-118-47661-1.
- ^https://www.ema.europa.eu/documents/scientific-guideline/draft-paracetamol-oral-use-immediate-release-formulations-product-specific-bioequivalence-guidance_en.pdf
Further reading[edit]
- Folkers G, van de Waterbeemd H, Lennernäs H, Artursson P, Mannhold R, Kubinyi H (2003). Drug Bioavailability: Estimation of Solubility, Permeability, Absorption and Bioavailability (Methods and Principles in Medicinal Chemistry). Weinheim: Wiley-VCH. ISBN3-527-30438-X.
- Amidon GL, Lennernäs H, Shah VP, Crison JR (March 1995). 'A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability'. Pharm. Res. 12 (3): 413–20. PMID7617530.
External links[edit]
- BCS guidance of the U.S. Food and Drug Administration
A microbiologist performing influenza research within a biosafety cabinet | |
| Acronym | BSC |
|---|---|
| Other names | Biological safety cabinet, microbiological safety cabinet |
| Uses | Biocontainment |
| Related items | Laminar flow cabinet Fume hood Glove box |
A biosafety cabinet (BSC)—also called a biological safety cabinet or microbiological safety cabinet—is an enclosed, ventilated laboratory workspace for safely working with materials contaminated with (or potentially contaminated with) pathogens requiring a defined biosafety level. Several different types of BSC exist, differentiated by the degree of biocontainment required. BSCs first became commercially available in 1950.[1]
- 2Classes
Purposes[edit]
The primary purpose of a BSC is to serve as a means to protect the laboratory worker and the surrounding environment from pathogens. All exhaust air is HEPA-filtered as it exits the biosafety cabinet, removing harmful bacteria and viruses.[2] This is in contrast to a laminar flow clean bench, which blows unfiltered exhaust air towards the user and is not safe for work with pathogenic agents.[3]:13[4] Neither are most BSCs safe for use as fume hoods.[2] Likewise, a fume hood fails to provide the environmental protection that HEPA filtration in a BSC would provide.[5] However, most classes of BSCs have a secondary purpose to maintain the sterility of materials inside (the 'product').
Classes[edit]
The U.S. Centers for Disease Control and Prevention (CDC) classifies BSCs into three classes.[3]:6 These classes and the types of BSCs within them are distinguished in two ways: the level of personnel and environmental protection provided and the level of product protection provided.
Class I[edit]
Class I cabinets provide personnel and environmental protection but no product protection. In fact, the inward flow of air can contribute to contamination of samples.[6] Inward airflow is maintained at a minimum velocity of 75 ft/min(0.38 m/s). These BSCs are commonly used to enclose specific equipment (e.g. centrifuges) or procedures (e.g. aerating cultures) that potentially generate aerosols. BSCs of this class are either ducted (connected to the building exhaust system) or unducted (recirculating filtered exhaust back into the laboratory).[3]:6
Class II[edit]
Class II cabinets provide both kinds of protection (of the samples and of the environment) since makeup air is also HEPA-filtered. There are five types: Type A1 (formerly A), Type A2 (formerly A/B3), Type B1, Type B2 and Type C1. Each type's requirements are defined by NSF International Standard 49,[3]:31 which in 2002 reclassified A/B3 cabinets (classified under the latter type if connected to an exhaust duct) as Type A2,[5] and added the Type C1 in the 2016 standard.[7] About 90% of all biosafety cabinets installed are Type A2 cabinets.[6]
Principles of operation use motor driven blowers (fans) mounted in the cabinet to draw directional mass airflow around a user and into the air grille - protecting the operator. The air is then drawn underneath the work surface and back up to the top of the cabinet where it passes through the HEPA filters. A column of HEPA filtered, sterile air is also blown downward, over products and processes to prevent contamination. Air is also exhausted through a HEPA filter, and depending on the Type of Class II BSC, the air is either recirculated back into the laboratory or pulled by an exhaust fan, through ductwork where it is expelled from the building. [8][citation needed]
The Type A1 cabinet, formerly known as Type A, has a minimum inflow velocity of 75 ft/min. The downflow air, considered contaminated, splits just above the work surface (the BSCs smoke split) and mixes with the inflow. This air is drawn, through ductwork, up the back of the cabinet where it is then blown into a positive pressure, contaminated plenum. Here, the air is either recirculated, through a HEPA filter, back down over the work zone, or exhausted out of the cabinet (also through a HEPA filter). Sizing of HEPA filters and an internal damper are used to balance these air volumes. This type is not safe for work with hazardous chemicals even when exhausted with a 'thimble' or canopy to avoid disturbing internal air flow.[3]:8–9
The Type A2 cabinet, formerly designated A/B3, has a minimum inflow velocity of 100 ft/min. A negative air pressure plenum surrounds all contaminated positive pressure plenums. In other respects, the specifications are identical to those of a Type A1 cabinet.[3]:9–11[5]
Type B1 and B2 cabinets have a minimum inflow velocity of 100 ft/min, and these cabinets must be hard-ducted to an exhaust system rather than exhausted through a thimble connection. Their exhaust systems must also be dedicated (one BSC per duct run, per blower). In contrast to the type A1 and A2 cabinets, Type B BSCs use single pass airflow (air that does not mix and recirculate) in order to also control hazardous chemical vapors. Type B1 cabinets split the airflow so that the air behind the smoke-split is directed to the exhaust system, while air between the operator and the smoke-split mixes with inflow air and is recirculated as downflow. Since exhaust air is drawn from the rear grille, the CDC advises that work with hazardous chemistry be conducted in the rear of the cabinet.[3]:10 This is complicated, since the smoke split (demarking the 'rear of the cabinet') is an invisible line that extends the width of the cabinet (approximately 10-14 inches from the front grille) and drifts as the internal HEPA filters load with particulate.[8]
The Type B2 cabinet (also known as a Total Exhaust BSC) is expensive to operate because no air is recirculated within.[3] Therefore, this type is mainly found in such applications as toxicology laboratories, where the ability to safely use hazardous chemistry is important.[5] Additionally, there is the risk that contaminated air would flow into the laboratory if the exhaust system for a Type B1 or B2 cabinet were to fail. To mitigate this risk, cabinets of these types generally monitor the exhaust flow, shutting off the supply blower and sounding an alarm if the exhaust flow is insufficient.[3]:10–11
The Type C1 BSC was borne out of necessity to control infectious material, chemical hazards, reduce operating costs and add flexibility in modern laboratories. The Type C1 moves air by mixing inflow air with the air in the columns of downflow air marked for recirculation. Air above a clearly delineated section of the work surface is drawn by a second internal fan where it is exhausted through a HEPA filter. The C1 differs from a Type A in that it can use this single pass airflow, and when installed in a ducted operating mode, can protect from hazardous chemistry, like the Type Bs. The C1 also differs from the Type B BSCs in several ways; (1) it does not require a hard connected, dedicated exhaust system and blower to operate, (2) pending a risk assessment, the BSC can run for an extended duration to increase operator protection during a remote exhaust system failure, and (3) Type C1 BSCs can run without being connected to an exhaust system at all.[9]
Class II cabinets are the commonly used cabinets in clinical and research laboratories.
Class III[edit]
The Class III cabinet, generally only installed in maximum containment laboratories, is specifically designed for work with BSL-4 pathogenic agents, providing maximum protection. The enclosure is gas-tight, and all materials enter and leave through a dunk tank or double-door autoclave. Gloves attached to the front prevent direct contact with hazardous materials (Class III cabinets are sometimes called glove box). These custom-built cabinets often attach into a line, and the lab equipment installed inside is usually custom-built as well.[3]:12–13
Ergonomics[edit]
Bcs Classification Of Drugs
Biosafety cabinets are used on a daily basis for hours. Besides protection of user and sample material, the human design factors (ergonomics) of the work become more and more important. This includes reduction of the noise level (for a more convenient working atmosphere), a height adjustable stand or stool (for optimized sitting position), panorama side windows (more light within cabinet), 10°angled front sash (enables better sitting position) as well as strong light sources (better view within cabinet) to improve the working conditions.
Ultraviolet lamps[edit]
The CDC does not recommend the installation of UV lamps in BSCs.[3]:12–13 The American Biological Safety Association supports this position, citing the safety risk to personnel, shallow penetration, reduced effectiveness in high relative humidity, and the frequent need to clean and replace the bulb.[10] UV lamps should not be used as a primary source of surface decontamination within a BSC.[11] However, these assertions have been formally disputed in at least one peer-reviewed article which points out that:[12]
- There is no cited basis for the need to remove dust and dirt from bulbs
- Properly functioning biosafety cabinets have very clean air so dust is less likely to build up
- Laboratories are generally air-conditioned which eliminates the concern over humidity inhibition of UV effectiveness
- With proper use UV exposure risk to users is very low
- UV disinfection is effective for germicide and virucide as well as inhibiting DNA contamination from PCR
- UV disinfection has the advantage of not leaving residues like physical disinfectants
- The relative safety and risks of UV versus other disinfection techniques (which also entail risks) should be considered
Maintenance and service[edit]
Cabinets need to be maintained on a regular schedule. During this certification check, the airflow and the filter capacities are verified. The filters have a limited lifespan - determined by the air quality within the laboratory space and the amount of particles and aerosols generated inside the BSC' work zone. As these filters load, the internal fan is required to do more work to push/pull the same volume of air through them. Newer cabinets measure the air flow constantly and self compensate fan performance to ensure constant volumes of air moving through the filters and the cabinet. If the flow drops below desired performance an audio and visual alarm will alert the operator. Changing the filter should be limited to trained persons as the filter is potentially contaminated. This can be done either after the cabinet has been decontaminated using a gaseous procedure (using formaldehyde, chlorine dioxide or vaporized hydrogen peroxide) or a 'bag-in/bag-out' procedure.
When an UV light is used, this lamp should be checked and changed as well. UV lights decrease in power over time, resulting in diminished disinfection of the working area.
Work practices[edit]
As with work on open bench tops, work performed within a BSC must be performed carefully and safely. To avoid contamination and the risk of personnel exposure, the CDC advises investigators to follow best practices to reduce and control splatter and aerosol generation, such as keeping clean materials at least 12 inches (30 cm) from aerosol-generating activities and arranging the work flow 'from clean to contaminated'.[3]:22 In particular, open flames, not necessary within the clean environment of a Class II or III BSC, cause disruption of the airflow inside.[3]:22 Once work inside a BSC has been completed, it is necessary to decontaminate the surfaces of the BSC as with other lab equipment and materials.[3]:24
When a BSC is serviced or relocated, including replacement of HEPA filters, it must be gas decontaminated. Gas decontamination involves filling the BSC with a poisonous gas, most commonly formaldehyde gas.[3]:25
See also[edit]
| Wikimedia Commons has media related to Fume hoods. |
References[edit]
- ^Wedum, A.G. (1969), 'The Detrick experience as a guide to the probable efficacy of P4 microbiological containment facilities for studies on microbial recombinant DNA molecules'; J Am Biol Safety Assoc;1:7-25.
- ^ abIowa State University (2005). 'Biosafety Cabinets'. Retrieved April 24, 2010.
- ^ abcdefghijklmnoU.S. Centers for Disease Control and Prevention; U.S. National Institutes of Health (2000). Primary Containment for Biohazards: Selection, Installation and Use of Biological Safety Cabinets(PDF). U.S. Centers for Disease Control and Prevention.
- ^University of Pennsylvania (November 6, 2009). 'Clean Benches vs. Biosafety Cabinets'. Retrieved April 24, 2010.
- ^ abcdThe Baker Company (2010). 'Introduction to Biological Safety Cabinets'. Retrieved April 26, 2010.
- ^ abDePalma, Angelo (October 7, 2009). 'Product Focus: Biological Safety Cabinets'. Lab Manager. Retrieved April 26, 2010.
- ^'3 Takeaways from the 2016 NSF/ANSI Standard 49 update - Labconco'. www.labconco.com. Retrieved 2017-05-30.
- ^ ab'Biosafety Cabinet No-Brainer - Labconco'. www.labconco.com. Retrieved 2017-05-30.
- ^'Biosafety Cabinet Gaps In Safety - Labconco'. www.labconco.com. Retrieved 2017-05-30.
- ^American Biological Safety Association (December 2000). 'Position Paper on the Use of Ultraviolet Lights in Biological Safety Cabinets'(PDF). Archived from the original(PDF) on October 11, 2010. Retrieved April 26, 2010.
- ^'Biosafety in Microbiological and Biomedical Laboratories'(PDF).
- ^Meechan, Paul; Christina Wilson (2006). 'Use of Ultraviolet Lights in Biological Safety Cabinets: A Contrarian View'. Applied Biosafety. 11 (4): 222–227.



